Cataract Surgery Recovery: Timeline, Tips, and What to Expect
Introduction
Modern cataract surgery reliably restores clarity, but the real story unfolds after you leave the operating room. Recovery is where small daily habits, smart safeguards, and timely check-ins combine to protect your new lens and fine-tune your vision. Knowing what to expect reduces stress, helps you spot normal milestones versus warning signs, and makes it easier to return to driving, work, and hobbies with confidence. This guide translates clinical steps into everyday actions—practical, steady, and grounded in typical timelines—so you can navigate the coming days and weeks with calm focus.
Outline
– Day 0 to Week 1: What Healing Looks Like Hour by Hour
– Weeks 2–4: Sharpening Vision and Easing Back into Routine
– Medications, Eye Drops, and Practical Home Care
– Potential Problems, Red Flags, and When to Call Your Surgeon
– Long-Term Eye Health After Cataract Surgery: Habits, Lenses, and Life
Day 0 to Week 1: What Healing Looks Like Hour by Hour
The first week sets the tone for safe, steady healing. Most procedures today use small incisions and ultrasound to remove the cloudy lens, followed by placement of a clear artificial lens. Immediately afterward, expect a shield over the eye and some blurriness—think of it as the lens settling into a new home. Many people notice brighter colors within hours, while others need a day or two for the fog to lift. Mild scratchiness, tearing, light sensitivity, and a feeling like something is in your eye are common and typically fade as the surface heals.
During the first 24 hours, rest is your main job. Keep the shield on as directed, especially during sleep, to avoid accidental rubbing. Use sunglasses outdoors because the dilated pupil and new lens can make light feel intense. A mild over-the-counter pain reliever is usually enough if you feel discomfort, but if pain is more than mild or worsens, it’s worth calling your surgeon. Many surgeons recommend a first check the same day or the next day to confirm pressure, alignment, and incision integrity; that visit is a good time to review drop schedules and clarify your activity plan.
Typical restrictions in Week 1 are about protecting the incision and preventing germs from entering the eye. That means avoiding swimming pools, hot tubs, and lakes; keeping soapy water out of the eye in the shower; and skipping heavy lifting or straining. Light walking is fine, and gentle household tasks are usually safe. Screens are not off-limits, but frequent breaks and artificial tears (if approved) help with dryness. Blinking often and following the 20-20-20 rule can reduce eye fatigue as your brain adapts to a sharper image.
It helps to separate “common and temporary” from “unusual and urgent” in these first days. Common: mild redness, halos around bright lights at night, a dry or gritty sensation, and fluctuating focus. Urgent: a sudden drop in vision, severe eye pain, increasing redness with thick discharge, or flashes and a curtain-like shadow. Having those categories in mind makes the early days clearer and less stressful.
Weeks 2–4: Sharpening Vision and Easing Back into Routine
By the second week, most people feel steadier and start noticing consistent improvements—contrast pops, whites look truly white, and small details on labels or dashboards become easier to pick out. Depth perception continues to recalibrate as swelling subsides and the new lens stabilizes. If you had one eye done first, it can feel like one camera has a different exposure setting than the other; that mismatched sensation typically fades as your brain fuses the images. Driving often resumes when vision in the operated eye meets local standards and glare feels manageable; confirm this at follow-up before getting behind the wheel.
Activity-wise, the arc bends toward normalcy. Many people return to desk work within 3–7 days, and by Weeks 2–4 they often handle regular schedules with sensible limits. Still, a few guardrails matter: keep weightlifting light to moderate; avoid dusty environments if possible; and continue to shield the eye during sleep if your surgeon advises it. Swimming and hot tubs usually remain off-limits until you’re cleared, as water exposure can carry microbes that raise infection risk. Outdoor exercise is welcome—think walking trails, stationary cycling, or easy hikes—with wraparound sunglasses for wind and UV.
Vision quality in this window depends partly on the lens design and your preexisting eye health. Monofocal lenses tend to give crisp distance with glasses often needed for near tasks, while multifocal or extended-depth lenses trade a bit of contrast for a wider range of focus. If astigmatism was corrected, you may notice sharper edges sooner, though night halos can linger longer as the brain adapts. Many clinics schedule a refraction around Week 3–4 to fine-tune temporary glasses if needed; your final prescription may wait until swelling and micro-adjustments settle.
A few practical cues help you judge readiness for tasks:
– Reading: If print swims, use stronger ambient light and larger fonts; expect improvement as the cornea clears.
– Screens: Increase text size and reduce glare; brief sessions with breaks work better than marathons.
– Driving at night: Only when glare feels predictable; keep windshields clean to reduce scatter.
– Work: Ramp up gradually; microbreaks keep dryness from stealing focus.
Overall, Weeks 2–4 mark the shift from “protecting” to “optimizing”—you’re still cautious, but you’re also reclaiming routines with more confidence.
Medications, Eye Drops, and Practical Home Care
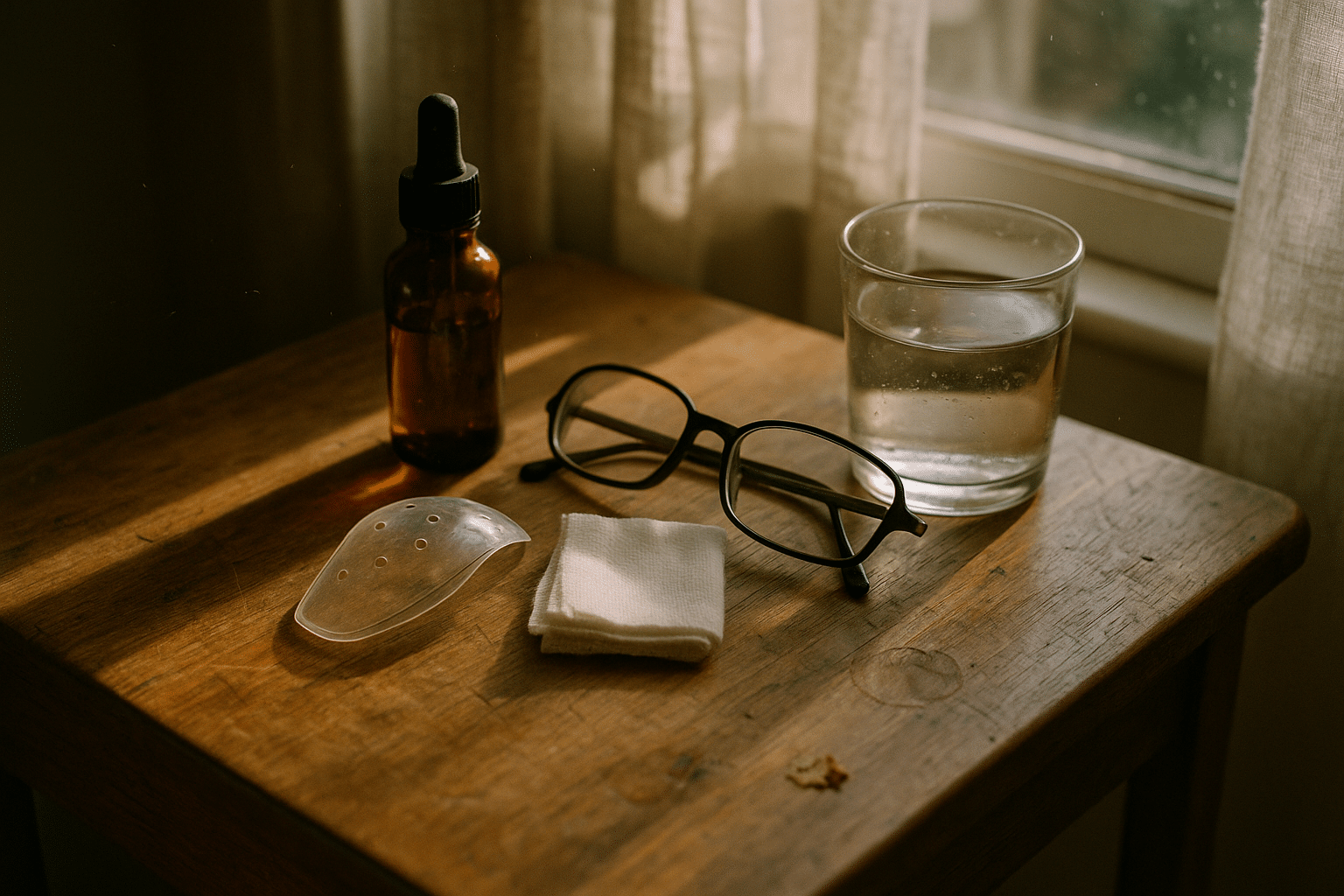
Postoperative eye drops do heavy lifting in recovery by lowering infection risk and controlling inflammation. A common plan includes an antibiotic for about a week and an anti-inflammatory (steroid and/or nonsteroidal) tapered over several weeks. Your exact schedule may differ, and following the written plan precisely matters more than any generic timetable. Wash hands before every application, avoid touching the tip to lashes or skin, and wait 5 minutes between different drops so each has time to absorb. If bottles look similar, color-code caps or store them in order of use to prevent mix-ups.
Dryness and fluctuating focus are frequent in the first month, partly from surface healing and partly from normal tear film changes. Preservative-free artificial tears, if approved by your surgeon, can smooth the visual surface and reduce scratchiness. A simple warm compress once or twice daily helps meibomian glands flow, supporting a more stable tear film; just keep the cloth clean and avoid pressing on the eye. Some people report more glare and halos initially; an anti-reflective lens coating on glasses and matte room lighting can make evenings more comfortable while neural adaptation proceeds.
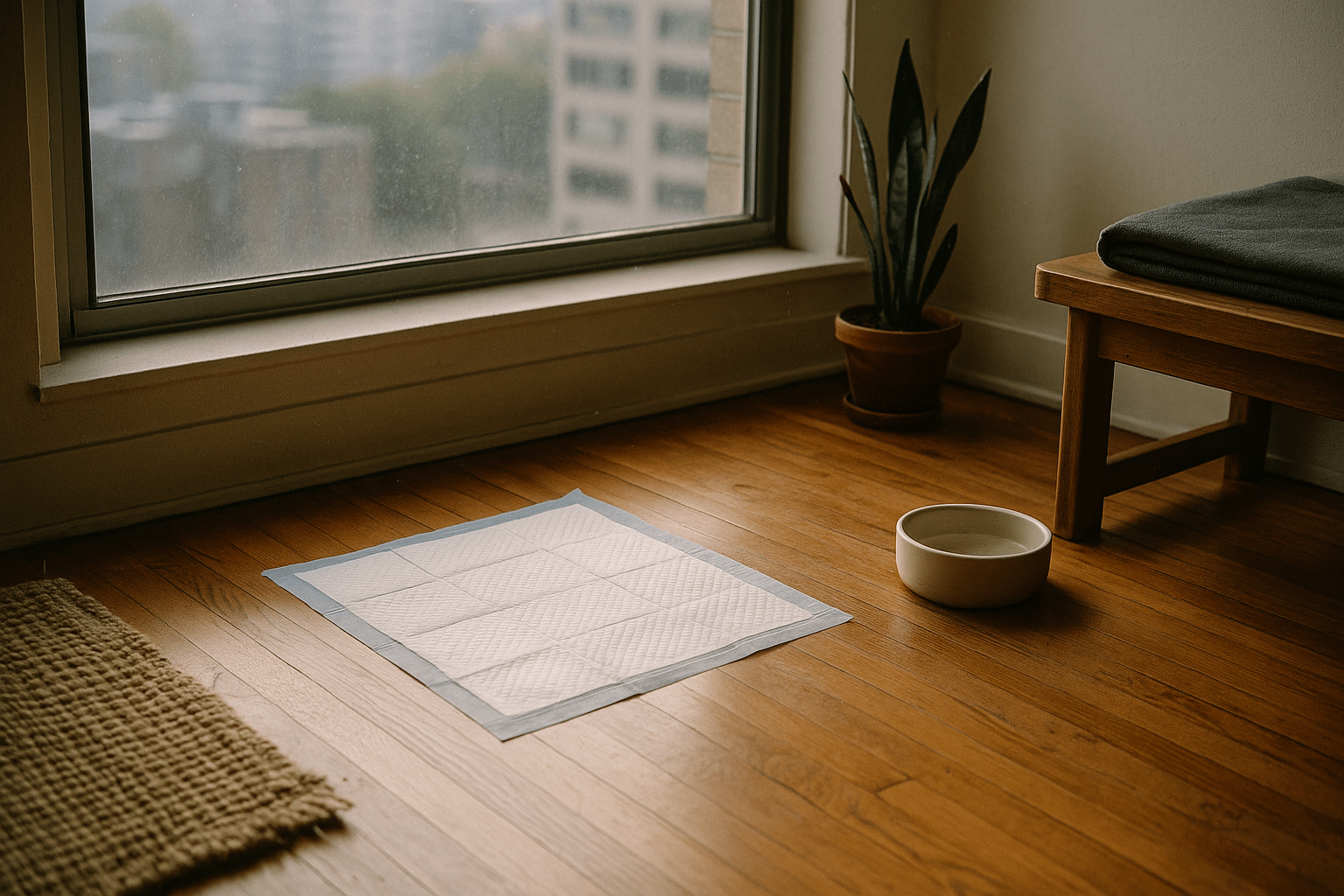
Home care is about preventing bumps in the road. Consider preparing a small “recovery kit” before surgery:
– Shield or protective glasses to reduce rubbing and accidental bumps.
– Preservative-free tears (if cleared), tissues, and a clean microfiber cloth.
– A calendar or phone reminders for drop timing and follow-ups.
– A bedside lamp with warm, diffuse light to reduce glare at night.
– A lightweight hat or visor for sunny walks to ease light sensitivity.
Nutrition and hydration support the eye’s microenvironment. A routine with leafy greens, colorful vegetables, omega-3-rich foods, and adequate water encourages a healthy tear film and general healing. While supplements can be helpful for some, introduce them only with your clinician’s approval. Sleep also matters; most people wear a shield for several nights to prevent rubbing, which can protect the incision and reduce morning dryness. If headaches crop up from new focusing demands, short breaks, gentle stretching, and a consistent sleep schedule often help.
Finally, track symptoms. A simple log—date, time, drops used, and any new sensations—makes follow-up visits more useful. Patterns such as afternoon blur relieved by tears, or halos that diminish week by week, tell a reassuring story; sharp deviations from your baseline are a signal to call.
Potential Problems, Red Flags, and When to Call Your Surgeon
Serious complications after cataract surgery are uncommon, but quick action matters when something feels off. The big concerns in the first days include infection, significant pressure spikes, and wound leakage. After the first week, inflammation that lingers or a sudden rise in floaters can signal issues that deserve prompt evaluation. Most people never encounter these problems, yet recognizing them helps you respond calmly and effectively if they do appear.
Use this plain-language checklist:
– Call urgently if vision drops suddenly, pain becomes moderate to severe, the eye becomes very red, or thick discharge appears.
– Seek same-day advice if you see flashes of light or a shadow like a curtain drifting across your vision.
– Report persistent nausea with eye pain, which can accompany a pressure rise.
– If halos are worsening rather than stabilizing after the first couple of weeks, mention it at your check.
Other scenarios are less dramatic but still worth attention. Some people develop temporarily elevated pressure from steroid drops; a quick measurement and a dosing adjustment can resolve it. A small percentage experience posterior capsule opacification months later, which makes vision hazy again; a brief in-office laser procedure can often clear the clouding and restore sharpness. If you notice decentering glare or edge reflections from the implant, describe when and where you see them (night driving, side lighting, reading lamps) so your clinician can assess whether it’s neural adaptation or something that needs correction.
Distinguishing normal healing from trouble gets easier when you track timing. Mild ache the first evening? Common. Light sensitivity and watery eyes in Week 1? Expected. Vision a touch fuzzy in the morning and clearer by afternoon? Often related to tear film. By contrast, any rapid change—especially if paired with pain or a shadow—deserves a same-day call. Recovery is a partnership: you monitor how you feel, and your care team interprets the signals.
To keep perspective, large studies report the vast majority of patients achieve meaningful improvement in visual function, with serious complications being rare. Keeping your appointments, using drops exactly as prescribed, and avoiding early exposure to contaminated water are the simplest ways to tip the odds even further in your favor.
Long-Term Eye Health After Cataract Surgery: Habits, Lenses, and Life
By the three-month mark, most people have settled into a stable prescription and comfortable routines. Many choose distance-focused glasses with readers for near tasks, while others use progressive lenses to bridge distances smoothly. If you received a multifocal or extended-depth implant, you may rely less on spectacles overall, though contrast in dim light can take longer to feel natural. Regardless of the lens type, protecting the ocular surface keeps vision clear: steady hydration, regular breaks, and blinking habits all play a role in maintaining a crisp image across the day.
Think holistically about long-term eye wellness. A few simple anchors go a long way:
– Sun protection: Quality sunglasses that block UV help the cornea and retina over the long haul.
– Environment: Reduce drafts and direct fan air; add a desktop humidifier during dry seasons.
– Work setup: Raise screens to eye level, boost font size, and use task lighting that minimizes glare.
– General health: Manage blood sugar, blood pressure, and sleep—each influences ocular comfort and clarity.
Lifestyle tweaks often pay off at night. Keep windshields and glasses spotless to cut glare scatter. Use warm, indirect home lighting, and position lamps to the side rather than directly behind your field of view. If halos around streetlights remain distracting, an anti-reflective coating and strategic route choices (better-lit streets, fewer oncoming high beams) can help while your brain continues adapting. For hobbies—gardening, woodworking, or pickleball—eye protection becomes a quiet habit: clear wraparound lenses outdoors and impact-rated shields for tools prevent the kind of bumps that can be costly.
Long-term follow-up doesn’t end after the final post-op visit. Annual dilated exams check implant position, eye pressure, and retinal health. If you notice creeping haze months or years later, bring it up; posterior capsule changes are common and usually fixable in a short visit. For those with preexisting conditions—dry eye, macular changes, or glaucoma—your maintenance plan may include extra visits or targeted therapies, all aimed at preserving the clarity you gained from surgery.
Most of all, enjoy the upgrade. People often describe the world after cataract surgery as brighter and truer to memory—autumn leaves regain their copper and gold, and distant ridge lines look freshly carved. Keeping that clarity is less about heroic effort and more about consistent, modest habits practiced over time.
Conclusion
Cataract surgery recovery is a series of small, steady steps: protect the eye, use drops faithfully, resume activities thoughtfully, and speak up quickly if something changes. If you follow your tailored plan, most days will look a little clearer than the day before. Keep the timeline handy, lean on simple tools like shields, sunglasses, and reminders, and partner closely with your care team. With patience and practical habits, the return to confident, comfortable vision becomes a routine you can trust.