Guide to Men’s Health Trackers and Wellness Gadgets
Why Men’s Health Trackers Matter—and How This Guide Is Organized
Men often wait for a wake-up call before acting on health, yet daily micro-decisions shape long-term outcomes. Health trackers and wellness gadgets translate invisible signals—heart rhythm, sleep regularity, movement patterns—into numbers you can coach. In randomized studies, activity wearables have been associated with higher step counts (often around a thousand extra per day) and modest gains in moderate-to-vigorous exercise, especially when paired with goals and feedback. That said, sensors are not diagnoses, and gadgets work only when paired with habits you’ll keep. Think of these tools as dashboards: they can illuminate the road, but you still drive.
Outline of this guide:
– Core sensors and how accuracy varies by activity, skin characteristics, and environment
– Sleep, recovery, and readiness: translating metrics into smarter rest and training
– Heart, stress, and metabolic monitoring: where consumer tech helps—and its limits
– Choosing a device: form factor, battery life, durability, privacy, and budget
– Building habits and reading your data without stress or obsession
Why this matters specifically for men: elevated risks for conditions such as sleep apnea, hypertension, and cardiometabolic disease often go under-detected in routine life. Gentle nudges—an elevated resting heart rate after poor sleep, an irregular rhythm alert during a quiet afternoon, a weekly report flagging sedentary streaks—can prompt earlier conversations with clinicians. Trackers can also support performance goals many men care about, from lifting consistency to half-marathon prep. But amid bold marketing claims, it’s essential to know what’s reliable, what’s experimental, and how to align features with the way you actually live.
In the pages ahead, we compare common categories—watches, bands, rings, connected scales, blood pressure monitors, and more—without fixating on hype. You’ll see where wrist-based optical sensors shine (steady-state runs, daily resting data) and where chest straps, cuffs, or lab tests remain the reference. We’ll also cover privacy and data control so your most personal information doesn’t wander. By the end, you’ll have a grounded plan to pick gear you’ll wear, interpret the numbers with confidence, and turn insights into steady progress.
Core Sensors, Signals, and Real-World Accuracy
Under the hood, most wearables rely on a familiar toolkit. Optical heart-rate sensors use photoplethysmography (PPG) to estimate pulse by shining light into tissue and reading changes in reflection. Accelerometers and gyroscopes infer steps, cadence, and body orientation. Barometers and altimeters estimate elevation gain. Global positioning systems track outdoor routes and pace. Additional modules—skin temperature, electrodermal activity, and blood oxygen saturation—round out the picture. Each sensor has strengths, caveats, and environmental quirks that shape its reliability.
Heart rate and heart-rate variability (HRV) are among the most referenced metrics. At rest and during steady cardio, modern optical sensors can be impressively close to chest-strap readings. During high-intensity intervals or strength training, wrist movement and grip tension can corrupt PPG signals, leading to lag or spikes. Practical tips improve results:
– Wear the device snug but not constrictive; loose straps cause bounce artifacts
– Position slightly above the wrist bone to reduce motion
– Warm up in cold weather to enhance peripheral blood flow
– Consider a chest strap for intervals or heavy lifts if precision matters
GPS performance depends on sky view and surroundings. In open areas, consumer GPS commonly lands within a few meters of true position; dense trees or tall buildings can introduce significant drift, affecting instantaneous pace and distance. Multi-band receivers and satellite augmentation can help, but route smoothing still matters for city runners. Altitude estimates blend barometric pressure (sensitive to weather) with GPS data; short, steep hills may be miscounted if sampling is sparse.
SpO2 sensors are generally most reliable at rest and at sea level; movement, cold extremities, and darker pigments or tattoos may reduce signal quality. Temperature trends are useful for relative changes—detecting shifts from your baseline—rather than absolute clinical values. Skin tone, hair, and tattoos can challenge optical readings; design improvements continue, yet minor bias persists in some scenarios. The takeaway: trust trends over single points, corroborate with how you feel, and use higher-fidelity tools—chest straps, lab tests, clinical cuffs—when decisions have stakes.
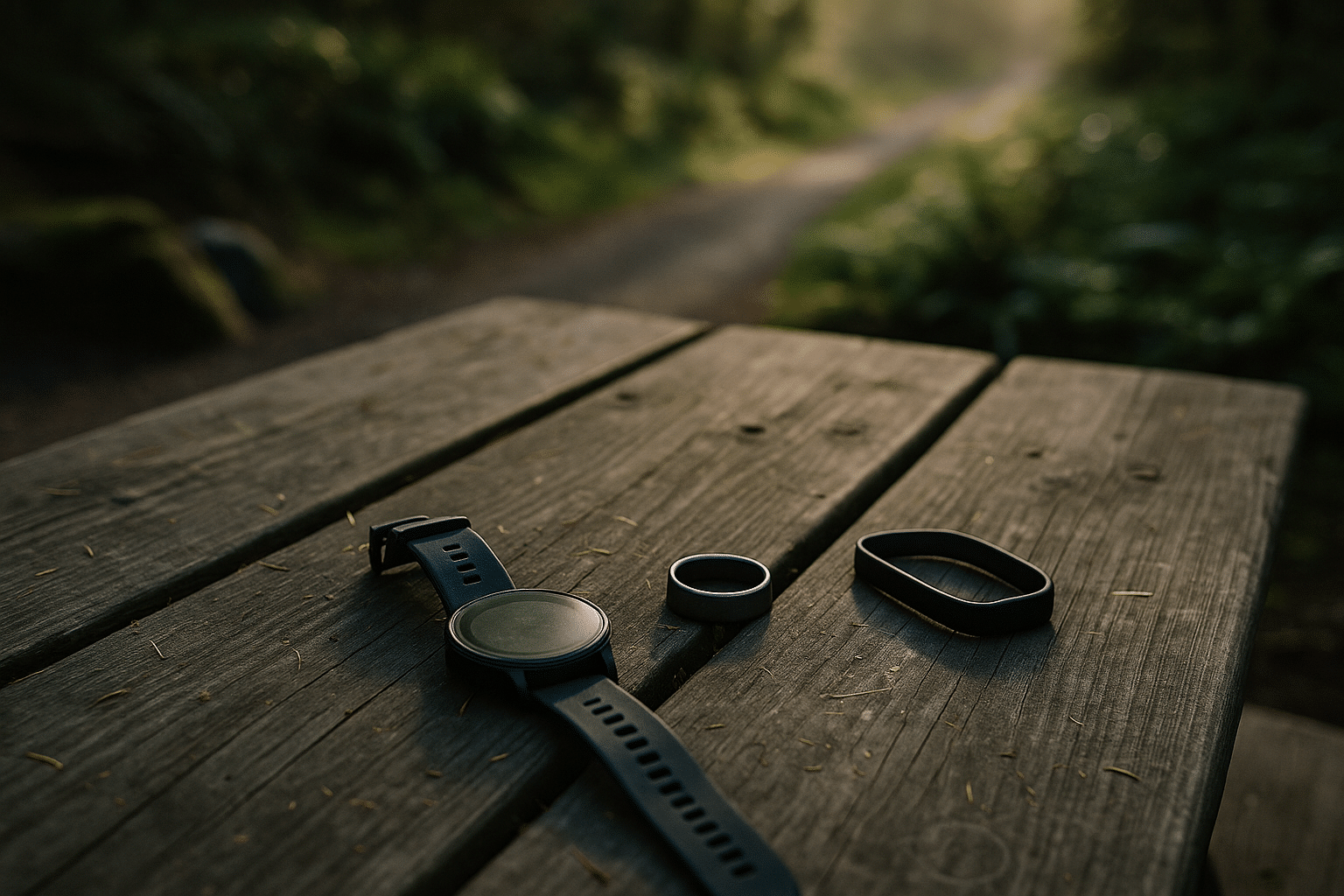
Form factor subtly shapes accuracy. Rings excel at nocturnal metrics thanks to stable finger perfusion; watches collect rich daytime movement and navigation data; slim bands trade screen size for comfort and long battery life. None is universally superior; instead, match the sensor’s context to your goal. For a desk-heavy week, gentle vibration nudges and standing reminders may outperform any advanced metric; for a trail weekend, barometer plus multi-GNSS support can make your elevation log believable.
Sleep, Recovery, and Readiness: Turning Night Data into Day Gains
Sleep tracking has matured from crude “toss-and-turn” tallies into layered profiles that include total sleep time, wake after sleep onset, efficiency, latency, and relative staging. Wrist and ring devices estimate stages using motion, heart rate, and sometimes temperature; they do not replicate lab polysomnography, but they can be remarkably consistent for personal trend tracking. What matters most is not a perfect stage label—it’s the pattern across nights: do you routinely cut sleep short midweek, or does travel wreck your bedtime? Those insights steer actionable tweaks.
Key signals many men find particularly useful:
– Resting heart rate (RHR): an elevated baseline after late meals, alcohol, or heavy training can flag under-recovery
– HRV: higher values (relative to your norm) often reflect parasympathetic dominance and better recovery capacity
– Skin temperature deviation: can hint at illness onset or circadian disruption
– Respiratory rate: stable for most, notable increases may correlate with stress, altitude exposure, or congestion
A practical “readiness” approach blends these into a simple question: should you push, maintain, or pull back? If your RHR is up, HRV is down, and sleep efficiency dipped below your usual, a lighter session or mobility work may beat a grind-it-out workout. Conversely, when trends look favorable, scheduling intervals or a heavy lift makes sense. For frequent travelers, stabilizing wake time, morning light exposure, and a short evening wind-down can restore rhythm faster than obsessing over nightly stage percentages.
Men carry a higher risk of sleep-disordered breathing across adulthood, and nighttime oxygen dips, loud snoring alerts, or unusually high respiratory rates warrant attention. Consumer wearables cannot diagnose apnea, yet recurring red flags combined with daytime sleepiness or morning headaches are a strong cue to seek a sleep study. Even without a diagnosis, simple tactics—side sleeping, consistent bedtimes, caffeine curfews, and moderating late alcohol—often register as improved efficiency and fewer nocturnal awakenings in your dashboard.
To make sleep data work for you, think experiments, not judgments. For two weeks, move dinner earlier and nudge bedtime 20 minutes sooner; watch how RHR, HRV, and sleep duration respond. Next, swap late screens for a short stretch or reading routine. Keep notes in your app or a paper log. After a month, you’ll likely see what your body already knew: small, repeatable changes compound, and the graph follows your habits—not the other way around.
Heart, Stress, and Metabolic Monitoring: Helpfulness and Boundaries
Heart-focused features have rapidly expanded, from irregular rhythm notifications to spot electrocardiograms using single-lead electrodes. In several peer-reviewed evaluations, single-lead consumer ECGs detected atrial fibrillation with high sensitivity and specificity under controlled conditions. Translation: a clear strip from a calm, seated reading can be informative; noisy readings during a run are less so. Any alert or concerning symptom—palpitations, chest discomfort, fainting—merits clinical follow-up regardless of what the watch shows.
Blood pressure is a different beast. Cuffless estimates derived from pulse transit time remain promising but variable; for decisions about hypertension, a validated upper-arm cuff is the practical standard. Some connected cuffs store and graph readings, enabling home monitoring protocols that clinicians increasingly recommend. Good practice includes taking two morning and two evening measurements for a week, seated, arm at heart level, and averaging the results.
Stress features lean on HRV, electrodermal activity, breathing rate, and sometimes temperature. These proxies won’t label your psychology, but they can nudge awareness: a streak of low HRV and frequent “high strain” tags might reflect stacked stressors—poor sleep, deadlines, hard training. Short interventions pay dividends:
– Two to five minutes of slow breathing (around six breaths per minute) can lift HRV acutely
– Walking breaks outdoors reset attention and mood
– Afternoon caffeine trims can reduce evening restlessness and bedtime latency
Metabolic tracking ranges from step counts and calorie estimates to VO2max approximations and even continuous glucose sensors. Energy expenditure from wearables remains a rough estimate; use it for trends, not as a strict calorie ledger. VO2max predictions from steady-state runs or walks are directionally helpful to gauge aerobic changes over weeks. Continuous glucose sensors can reveal how different breakfasts or late dinners influence your curve, though readings may vary by sensor and placement. For individuals without diabetes, the point is behavioral feedback, not disease management; discuss sustained anomalies with a professional.
A final note on context: lab-grade tools exist for a reason. Field data is complementary, offering frequency and convenience rather than hospital-level precision. Blend both worlds wisely. Annual checkups, blood panels, and, when indicated, formal screening coexist well with daily wearable data. Think of your gadgets as scouts—not generals—reporting back so you can make the next informed move.
Choosing the Right Device: Form Factor, Battery, Durability, and Privacy
Start with your routine, not the spec sheet. If you prefer analog watches at work, a slim band that disappears under a cuff may see more wear than a chunky multisport watch. If navigation, trail running, or open-water sessions matter, a robust watch with reliable satellite tracking and water resistance becomes compelling. Rings excel at passive, around-the-clock comfort and sleep fidelity. Connected scales, upper-arm cuffs, and simple chest straps quietly enhance the core trio by adding objective checkpoints.
Consider these practical dimensions:
– Battery life: rings often last 4–7 days; watches can span 1–10 days depending on GPS use; slim bands may hit a week or more; chest straps rely on coin cells for months
– Displays and controls: always-on screens aid quick glances, while fewer widgets extend runtime; tactile buttons trump touch in sweat or rain
– Durability: look for scratch-resistant glass, metal or reinforced polymer cases, and bands you won’t mind scuffing
– Water and dust: swim-friendly ratings and sealed ports matter for pool time and sandy weekends
– Comfort: lighter devices promote adherence; try varied band materials if skin gets irritated
Data handling should be part of your selection criteria. Scan for clear privacy policies, the ability to export your data (CSV or similar), and granular consent over sharing with third parties. Ask whether you can use the device in a limited mode without constant cloud sync and whether two-factor authentication is available. If you plan on switching ecosystems later, portability matters—open formats and standards reduce lock-in.
Budget can be optimized by prioritizing one anchor device and one validator. For example, pair a mid-range watch or ring for everyday tracking with a validated upper-arm cuff for monthly blood pressure snapshots; add a basic chest strap for interval accuracy. That trio covers most health bases without chasing every new sensor. For lifters, rep counting and rest timers may matter more than top-tier GPS. For desk-bound schedules, gentle movement nudges and sleep consistency often deliver the biggest return.
Try a reality check before buying: imagine your next seven days. Will you charge nightly or prefer weekly? Do you want post-run maps or just a step streak? Are you willing to wear jewelry overnight, or do you yank it off by instinct? Honest answers narrow the field to devices you’ll actually use—because the most capable tracker is the one that lives on your body, not in a drawer.
From Numbers to Habits: Making Data Actionable Without Obsession
Owning a tracker can feel like adopting a tiny coach and a tiny critic at once. The secret is to script behavior, not chase perfect metrics. Use implementation intentions: “If it’s 12:30, I take a brisk 10-minute walk,” or “If my evening HRV drops below my weekly median, I swap tomorrow’s intervals for an easy spin.” These simple rules turn dashboards into decisions without draining willpower.
Build a weekly cadence:
– Sunday: set three process goals (steps, bed window, two strength sessions)
– Midweek: five-minute audit—what friction can you remove tomorrow?
– Friday: look for trendlines, not trophies; celebrate adherence, not raw numbers
– Monthly: run a mini-experiment (new bedtime, different warm-up, lighter dinner) and compare baselines
Avoid common traps. Don’t let calorie estimates dictate eating to the decimal; they are rough. Resist late-night doomscrolling in the name of “sleep research.” Beware confirmation bias—when you feel great after a gentle week, let the data update your beliefs about recovery, not the other way around. If a metric becomes a stressor, hide it for a while; most apps let you customize views. Remember, fitness improves from stimulus and recovery in balance; the graph is a mirror, not a mandate.
Men juggling work, family, and training benefit from tiny anchors that survive chaos. Keep a resistance band near the desk, a pair of shoes by the door, and a standing calendar block for movement. Set charging rituals that fit your flow—perhaps during a shower or commute—so dead batteries never derail momentum. Share a weekly goal with a friend; social accountability beats yet another notification.
Finally, connect the dots to your values. Lower resting heart rate and steadier sleep are not just numbers—they translate to clearer thinking at 3 p.m., more patience with kids, and better weekends on the trail or court. When the data supports the life you want, adherence follows naturally. Use tech to notice patterns, take small steps, and keep going; over months, the quiet compounding becomes hard to miss, and the habits outlast the hardware.
Conclusion: A Practical Path for Men Navigating Health Tech
Trackers and wellness gadgets can be powerful allies when they match your routine, respect your privacy, and reinforce habits you’ll keep. Choose a comfortable form factor, trust trends over single points, and validate critical decisions with clinical tools when needed. Focus on three anchors—daily movement, consistent sleep, and regular strength—and let the sensors support, not control, your choices. With that mindset, the numbers become a compass, and your actions draw the map.


