Home Remedies for Fatty Liver: Evidence-Informed Lifestyle Tips
Outline
– Food patterns and a liver-friendly plate
– Movement and weight management at home
– Smarter drinks and alcohol guidance
– Herbs and supplements: what helps and what to skip
– Sleep, stress, and daily habits that protect your liver
Introduction
Fatty liver is increasingly common worldwide, largely tied to excess body fat, insulin resistance, and modern eating patterns. Left unchecked, it can progress from simple fat accumulation to inflammation and scarring over years. The encouraging news: daily choices at home—how you eat, move, sleep, and manage stress—can meaningfully shrink liver fat and improve lab markers. No single trick works in isolation; steady, combined habits deliver the most dependable gains. The sections below translate evidence into doable steps, highlight pitfalls to avoid, and keep the focus on practical routines rather than quick fixes. Always speak with a qualified clinician for personal guidance, especially if you have diabetes, are pregnant, or take prescription medications.
Liver-Friendly Eating: Build a Plate That Works Every Day
Your liver is the quiet night‑shift worker sorting nutrients and toxins while you sleep. It thrives when meals are predictable, fiber‑rich, and light on added sugars and refined starch. Studies suggest that losing 5–10% of body weight can substantially reduce liver fat, with about 10% linked to greater odds of improving inflammation and even fibrosis. You don’t need a complicated plan: a modest calorie deficit, smart carbohydrate quality, and steady protein often suffice. Think “pattern,” not perfection.
Start with a Mediterranean‑style, plant‑forward pattern: vegetables, fruits, legumes, whole grains, nuts, seeds, herbs, and mostly unsaturated fats. Replace refined carbohydrates (white bread, pastries, sugary cereals) and sweetened snacks with fiber‑dense choices. Aim for roughly 25–35 grams of fiber per day to temper insulin spikes and help reduce liver fat. Choose fats from olives, nuts, seeds, and fish, while trimming sources heavy in saturated fat. Protein—both plant and lean animal—helps control appetite and supports the muscle you need for glucose control.
Try this simple plate formula most days:
– Half non‑starchy vegetables (leafy greens, tomatoes, cruciferous veg)
– One quarter protein (beans, lentils, tofu, eggs, fish, or lean poultry)
– One quarter intact whole grains or starchy veg (oats, barley, quinoa, potatoes with skin)
– A thumb of healthy fat (olive oil drizzle, a few nuts or seeds)
Flavor with vinegar, citrus, spices, and herbs instead of sugar‑heavy sauces. Cook with methods that require less oil—roasting, steaming, grilling—yet keep meals satisfying with textures and spices.
Two homey ideas:
– Skillet beans and greens: sauté onion and garlic in a little olive oil, add cannellini beans, chopped kale, lemon, and chili flakes; serve over barley.
– “Rainbow bowl”: roasted carrots and cauliflower, chickpeas, cucumber, cherry tomatoes, and a spoon of yogurt with herbs over quinoa.
Be mindful with fruit: whole fruit is fiber‑rich and filling; juice concentrates sugar and can nudge liver fat upward. Keep sweets for occasional treats, and watch creeping calories from nuts, oils, and sauces. Aim for progress, not absolutes; a few upgraded meals each week add up quickly.
Move More, Sit Less: Home Fitness That Targets Liver Fat
Exercise is a direct line to a lighter, less stressed liver. Even without weight loss, consistent aerobic activity can lower liver fat, with some trials reporting meaningful reductions when people reach 150–300 minutes of moderate activity per week. Add two or three days of resistance training to build and preserve muscle, which acts like a glucose sponge and improves insulin sensitivity. You don’t need a gym; your living room, stairs, and a pair of resistance bands can cover the essentials.
Blend movement types for complementary benefits:
– Moderate aerobic: brisk walking, dancing, cycling on a stationary bike—target 30–45 minutes most days.
– Vigorous bursts: short intervals of faster walking or jogging for 20–60 seconds sprinkled into moderate sessions, repeated 6–10 times.
– Resistance work: squats, push‑ups (wall or floor), rows with bands, hip hinges, and presses; 2–4 sets of 8–12 reps.
– Flexibility and core: yoga‑style flows, planks, and hip mobility drills for posture and back health.
A practical weekly plan might include four days of brisk walking, two short interval sessions layered onto those walks, and two full‑body strength days. On busy weeks, ten‑minute “exercise snacks” stacked across the day can deliver similar totals.
Sedentary time matters. Long sitting spells drive insulin resistance, independent of workouts. Set a timer to stand and move for 2–3 minutes every 30–45 minutes: march in place, climb a flight of stairs, or do 15 body‑weight squats. Post‑meal walks—10 to 15 minutes—can blunt glucose spikes and are surprisingly potent for liver and metabolic health.
Measure what you can manage: a step count of 7,000–10,000 per day often correlates with better metabolic markers. If that sounds high, add 1,000–2,000 steps to your current average and build gradually. Keep the vibe friendly and doable: music you love, a doorway pull‑up bar, a mat in plain sight, and a calendar where you check off workouts. Momentum—more than intensity—is the home remedy that keeps paying dividends.
Smarter Drinks: Hydration, Coffee, Tea, and Alcohol Clarity
Sips shape liver health more than most people realize. Sugary drinks deliver swift fructose loads that funnel straight into liver fat production, while thoughtful choices can nudge the opposite direction. Anchor your day with water and unsweetened beverages, and be cautious with juice, energy drinks, and sweetened coffees or teas. A simple target is 6–10 cups of fluid daily, mostly water, adjusted for climate and activity level.
Coffee, without heavy sugar or cream, is linked in observational studies to lower risks of liver fibrosis and cirrhosis. Two to three cups a day may be a reasonable range for many adults, barring sensitivity to caffeine, pregnancy, or reflux. Tea—especially green or black—adds polyphenols with potential metabolic benefits; again, the advantage fades when sugar piles on. Be wary of concentrated green tea extracts in supplements; rare cases of liver injury have been reported with high doses, whereas brewed tea is far gentler.
Practical swaps at home:
– Replace afternoon soda with sparkling water, a squeeze of citrus, and mint.
– Brew a pot of unsweetened tea to chill for the week; add sliced ginger for bite.
– If you enjoy coffee, learn to like it with milk alternatives or plain; reserve sweetened versions for special occasions.
– For a hint of sweetness, try cinnamon or vanilla in beverages rather than sugar.
Alcohol deserves careful thought. While some people drink moderately without immediate lab abnormalities, alcohol can worsen fat accumulation and inflammation, particularly when metabolic risk factors are present. If you have fatty liver, many clinicians recommend avoiding alcohol; at minimum, discuss limits with your healthcare professional and follow national guidelines if you do drink. “Weekend only” binges are especially unkind to the liver. If social rituals revolve around drinks, build new cues: flavored seltzer in a stemmed glass, alcohol‑free bitters, or a tart shrub diluted with plenty of water. Your liver will notice the difference, quietly and quickly.
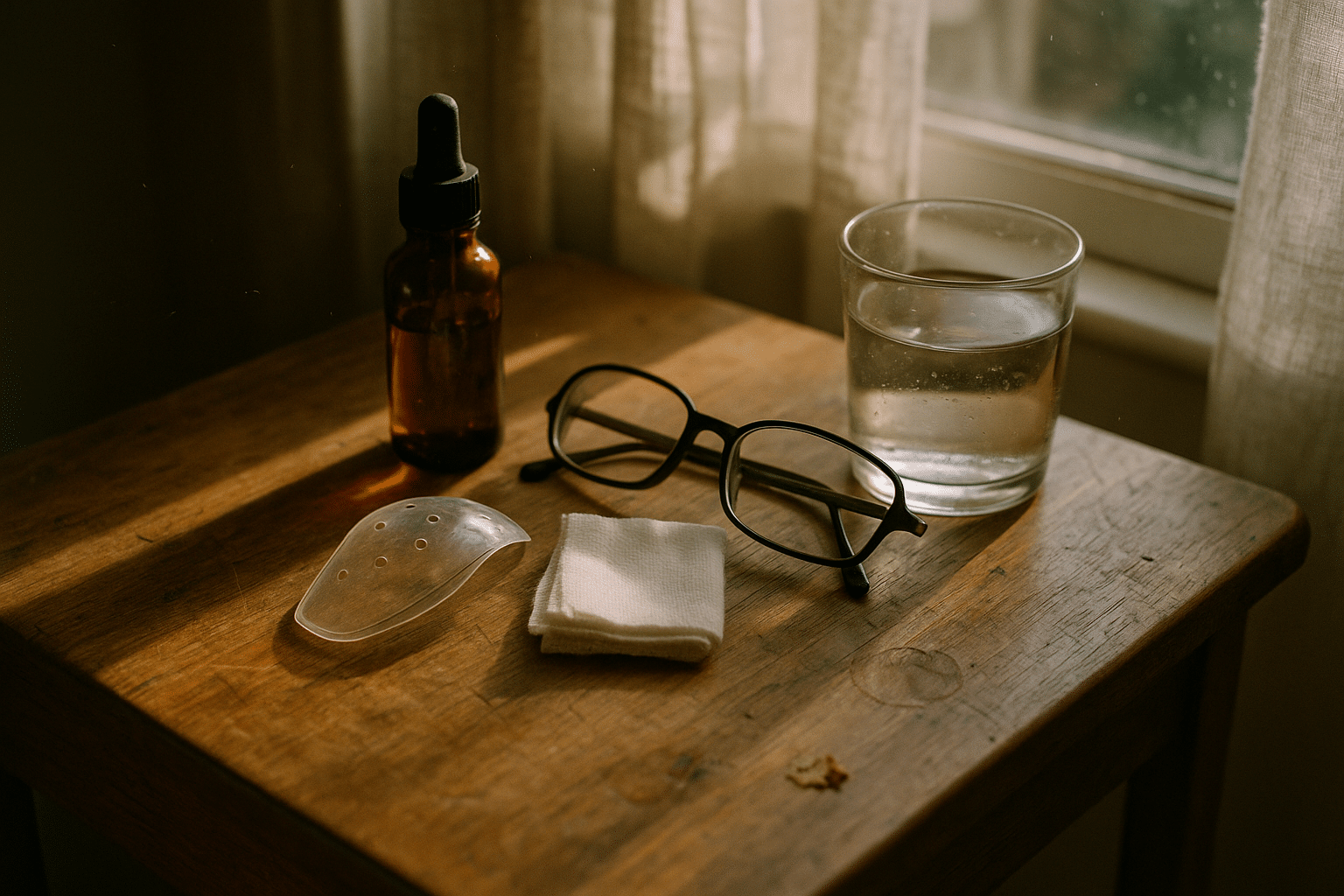
Herbs and Supplements: Sorting Signal from Noise
Most improvement in fatty liver comes from food patterns, movement, sleep, and weight management. Still, many people ask about pills and powders. The evidence is mixed, and quality control varies widely, so approach supplements as optional helpers, not center stage. Always consult a clinician and pharmacist if you take medications, have underlying conditions, or are pregnant or nursing.
What current research suggests:
– Vitamin E: In some adults without diabetes and with biopsy‑confirmed inflammatory fatty liver, 800 IU daily has improved liver enzymes and certain histologic features under medical supervision. Potential risks include bleeding tendency at high doses and signals for prostate risk in some studies; discuss thoroughly with a clinician.
– Omega‑3 fatty acids: Helpful for lowering high triglycerides and may reduce liver fat, though evidence for reversing scarring is limited. Typical studied intakes range around 2–4 grams of combined EPA/DHA daily. Can interact with blood thinners.
– Curcumin (from turmeric): Small trials report modest drops in liver enzymes and fat on imaging; absorption varies and high doses may cause gastrointestinal upset. Choose standardized products if advised by a clinician.
– Silymarin (milk thistle): Laboratory and some human data hint at antioxidant benefits, but clinical results are inconsistent; generally well tolerated, yet product potency varies.
– Berberine: May improve glucose and lipid profiles; interactions with many drugs are possible, including those affecting the liver’s enzyme systems.
– Green tea extracts: Concentrated forms have been linked, in rare cases, to liver injury; brewed tea is generally a safer option.
– Apple cider vinegar: Popular online, but robust evidence for fatty liver is lacking; its acidity can erode teeth and irritate the esophagus if not diluted.
Red flags to avoid:
– “Detox” cleanses or extreme fasts that promise rapid fat melting; they can cause dehydration, electrolyte imbalances, and rebound overeating.
– Proprietary blends with undisclosed amounts of active ingredients.
– Imported products without third‑party testing for contaminants.
If you and your clinician opt to trial a supplement, set a clear goal (for example, triglycerides or liver enzymes), track for 8–12 weeks, and reassess. Supplements should support, not distract from, the lifestyle foundation that does the heavy lifting.
Sleep, Stress, and Daily Routines: Quiet Levers with Big Impact
Sleep and stress may feel intangible, yet they steer hormones that control appetite, insulin sensitivity, and fat storage in the liver. Aim for 7–9 hours of sleep nightly with a consistent schedule, dim lights before bed, and a cool, quiet room. If you snore loudly, gasp at night, or feel unrefreshed despite plenty of time in bed, talk to a clinician about screening for sleep‑disordered breathing; treating it can meaningfully improve metabolic health.
Circadian rhythm matters for the liver. Many people find that shifting more calories earlier in the day—especially protein and fiber at breakfast and lunch—improves energy and eases evening cravings. Early time‑restricted eating (for example, meals within an 8–10 hour window ending by late afternoon) has shown promising improvements in glucose and liver enzymes in small studies; it is not suitable for everyone, including some people with diabetes, during pregnancy, or those with a history of disordered eating. If you try it, do so cautiously, prioritize nutrient‑dense meals, and get professional input.
Stress chemistry tugs on the liver through cortisol and adrenaline. Keep it practical:
– Insert brief breathing breaks: 4 seconds in, 6 out, for 2 minutes, three times daily.
– Take a 10‑minute outdoor “reset” after work to lower stress before dinner.
– Try gentle movement in the evening—stretching, a slow flow—to improve sleep onset.
Micro‑habits like these create calm without overhauling your schedule. Meanwhile, reducing long sitting stretches helps: set a “stand and stroll” cue every 30–45 minutes, and add a short post‑meal walk to tame glucose spikes.
Home organization smooths the path. Stock vegetables, beans, whole grains, eggs, yogurt, nuts, frozen berries, herbs, and spices. Prep two batch‑cooked items each weekend—perhaps a pot of lentils and a tray of roasted vegetables. Keep a water bottle visible. Write two SMART goals for the week (Specific, Measurable, Achievable, Relevant, Time‑bound), such as “walk 20 minutes after lunch Monday–Friday” or “include vegetables at two meals daily.” Invite a friend or family member to join you. Progress compounds when your environment nudges you in the right direction.
Conclusion: A Realistic Roadmap for Your Liver
Fatty liver changes slowly, for better and for worse. That’s an advantage—you have time to steer. Focus on a steady eating pattern rich in plants and fiber, regular movement with some strength work, mindful beverages, adequate sleep, and calm routines. Consider supplements only as side notes and only with professional advice. Choose two actions to start this week, track them, and build from there. Small, well‑kept promises to yourself are the most reliable home remedy your liver could ask for.