Smartwatch Glucose Monitoring: Benefits and Considerations
Introduction and Outline: Why Glucose on the Wrist Matters
Glucose numbers influence energy, focus, mood, and long-term health. Yet the moments when you most need to know your level—during a commute, before a meeting, after a workout—are often the moments when pulling out a phone or meter feels inconvenient. Smartwatch glucose monitoring meets that reality with a quick glance and a gentle tap on the wrist, putting timely information in your natural line of sight. While the watch rarely measures glucose directly, it serves as a companion that amplifies access to data, nudges better decisions, and lowers the friction of daily management. The goal is not to replace clinical care or foundational tools, but to create a calmer, more informed everyday experience where numbers are visible, understandable, and actionable.
This article unfolds in five parts, beginning with an overview and then diving into how the technology actually works, where it delivers value, and what to consider before adopting it. To set expectations, smartwatch monitoring should be viewed as an interface: it displays and contextualizes glucose information, often sourced from a continuous sensor or manual logging. With that frame, the benefits—timely alerts, trend awareness, and behavioral support—become clearer, as do the limits—accuracy boundaries, data lag, and privacy responsibilities. Think of your watch as a dashboard: it is only as meaningful as the engine behind it and the driver’s choices ahead.
Here is the outline we will follow to keep the journey clear and practical:
– How smartwatch glucose monitoring works today, including data sources, signal limits, and the state of non-invasive research.
– Health and lifestyle benefits, from alerting and trend insight to behavior change and collaboration with clinicians.
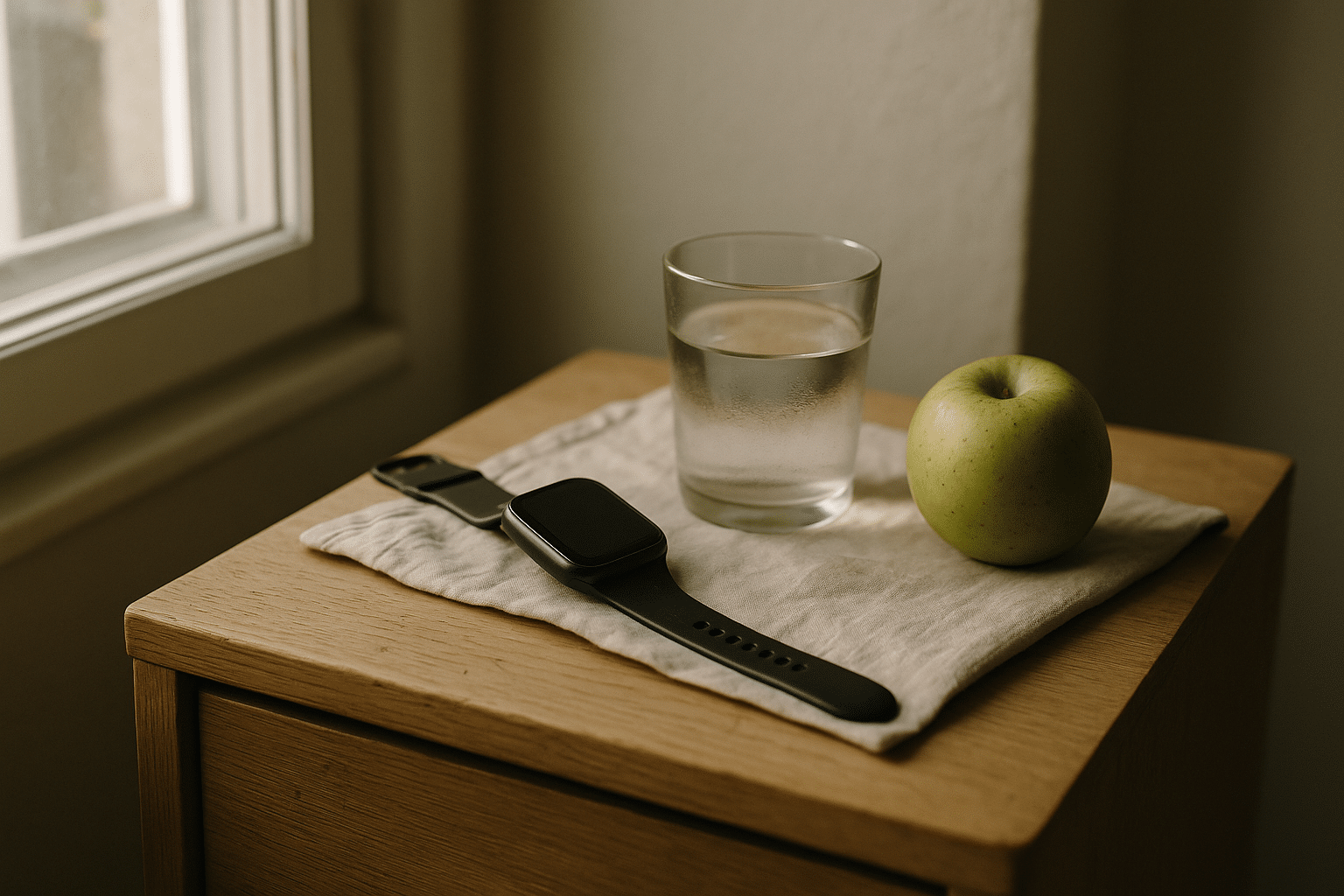
– Everyday usability: what alerts feel like in real life, how context from sleep and activity helps, and when the watch beats the phone.
– Considerations and safety: accuracy nuances, skin and battery issues, privacy, cost, and compatibility.
– Conclusion and a simple checklist to choose a setup that matches your routine and goals.
As you read, remember that individual needs vary. People using insulin, those relying on oral medications or diet, and those exploring preventive wellness will not use the same alerts or targets. The common thread is accessibility: when glucose information is easy to see and interpret, it invites small, timely adjustments that add up. That is the quiet power of the wrist—less fuss, more insight, and decisions made in the flow of life.
How Smartwatch Glucose Monitoring Works Today
Most smartwatches do not directly measure blood glucose. Instead, they extend access to data generated elsewhere. The two dominant sources are continuous glucose monitoring (CGM) sensors placed on the body and manual entries from fingerstick meters or meal/activity logs. The watch becomes a window—surfacing current readings, alarms, and trend arrows without requiring you to unlock a phone or carry a dedicated receiver. This is meaningful for daily comfort and for safety: subtle wrist vibrations can notify you of rapid drops or sustained highs in places where sound would be disruptive or a phone hard to reach.
Technically, CGM systems estimate glucose from interstitial fluid, not blood. That distinction matters: interstitial readings typically lag behind blood values by roughly 5–10 minutes, sometimes more during rapid changes. This lag is inherent to fluid movement and sensor chemistry, and it explains why trend information is as important as the current number. A downward arrow with a moderate reading may warrant faster attention than a static higher number that is drifting toward target. The watch excels at conveying this “direction”, which is critical context for decisions on food, activity, or medication under the guidance of a care plan.
What about non-invasive watch-based glucose? Research continues into optical, electrical, and sweat-based measurements, but fully wrist-only, non-invasive glucose monitoring cleared for medical decision-making is not widely available. Most consumer optical sensors on watches—such as those used for heart rate or blood oxygen estimation—do not measure glucose. When you see wrist devices referencing glucose, they are typically showing data relayed from a sensor or from user input, then layering it with other watch data like heart rate, steps, or sleep stages to provide context.
In practical terms, this means setup includes pairing a compatible app, granting permissions, and deciding which watch complications or tiles display glucose metrics. Accuracy depends primarily on the original data source and calibration requirements, if any. The watch adds convenience, discretion, and context—not magic. A helpful mental model:
– Data source: sensor and/or manual logging
– Transport: phone app or direct watch connection
– Display: numbers, trend arrows, and alerts
– Action: small, timely decisions aligned with a clinician-approved plan
Finally, remember that medical decisions should follow your healthcare provider’s advice. The watch is a tool for awareness and adherence. It can improve situational awareness, but it is not a substitute for professional guidance, lab testing, or emergency care.
Health and Lifestyle Benefits Backed by Evidence
The strongest value of smartwatch glucose monitoring lies in behavior and timing. Because the watch is always with you, it turns glucose from a sporadic check into a living signal you notice throughout the day. This is not just about a number; it is about understanding patterns and responding early. Clinical research on real-time CGM—whose data the watch often displays—has consistently linked greater visibility with improved time in range and reductions in hypoglycemia compared with traditional self-monitoring alone. Results vary by population and therapy, but the direction is clear: more timely feedback supports better self-management.
On the wrist, that feedback becomes effortless. Haptic cues deliver alerts even when your phone is in a bag or on a desk. Trend arrows help you choose a snack, a walk, or a pause before driving. Over weeks, these micro-decisions compound. People often report less anxiety because they do not need to wonder; they can glance and confirm. That reduction in mental load is difficult to quantify, yet it shows up in adherence: when information is accessible and non-intrusive, you are more likely to act on it. The watch also helps separate signals from noise: pairing glucose with sleep and activity patterns can highlight why the same meal behaves differently after a late night or a long run.
For those collaborating with clinicians, smartwatch-facilitated monitoring adds structure to conversations. Instead of recalling guesses, you can discuss clear episodes:
– Morning rises following shortened sleep
– Post-exercise dips after intense intervals
– Late-afternoon climbs during prolonged sitting
These grounded examples support tailored adjustments to nutrition, timing, or medication under medical supervision. In addition, routine exposure to trend information teaches the language of glycemic variability. Rather than chasing highs and lows reactively, you learn to anticipate and smooth the curve. While numbers still matter—time in range, glucose management indicator, variability—they become part of a broader story about habits, recovery, and stress. The watch is the narrator that keeps the story moving, one nudge at a time.
For individuals not on glucose-lowering medications, wrist-based visibility can still support healthier routines. It encourages mindful eating, movement after meals, and attention to sleep quality, all of which influence metabolic health. The goal is not perfection; it is steady, informed progress with tools that reduce friction and increase clarity.
Everyday Usability: Alerts, Context, and Real-World Scenarios
Usability decides whether any tool becomes a habit. Smartwatch glucose monitoring earns a place on the wrist by being quiet when you are in range and insistent when you are not. The haptic tap that gets your attention on a train, the subtle glance in a meeting, the pre-run check at a trailhead—these micro-interactions make the difference between intention and action. Compared with phone-only alerts, watch notifications are harder to miss and easier to triage discreetly. The device is on your skin, so you feel the message rather than hear it. When paired with glanceable complications, you can confirm status in a second without breaking stride.
Context is the other half of usability. The watch already tracks activity, heart rate, and sleep stages, and those signals can explain why your glucose behaves differently day to day. A steady post-breakfast rise after a short night is a different story than the same rise after a long walk. Linking events to patterns transforms management into learning. Over time, you can adjust meal timing, plan preemptive snacks for workouts, or schedule brief walks after larger meals. Convenience fuels adherence: when tools reduce effort, people use them longer.
Consider these real-world scenarios to illustrate the contrast with phone-only setups:
– Commuter: A gentle wrist buzz warns of a rapid drop. You step off, grab a small snack, and avoid a stressful low on a crowded bus.
– Athlete: Mid-run, a quick glance shows a downward trend; you sip carbs and keep your pace instead of stopping to unlock a phone.
– Parent or caregiver: Discreet check during a school event helps you stay present without repeated phone checks.
– Shift worker: Overnight alerts come through even when your phone is in a locker, making the environment safer and calmer.
Battery life and charging routines matter too. A watch that mirrors glucose should be charged daily at predictable times, like during a shower or desk work, to avoid gaps. Configuring focus modes, alert thresholds, and quiet hours aligns the system with your life rather than the other way around. And while the watch streamlines access, the phone app remains important for deeper review, log entries, and data sharing. Together, they form a layered system: wrist for awareness, phone for analysis, and clinician for guidance.
Conclusion: Considerations, Safety, and Choosing a Setup That Works
Smartwatch glucose monitoring is powerful, but it comes with responsibilities. First, accuracy depends on the underlying source. Interstitial fluid readings can lag during rapid changes; sensor placement, hydration, pressure on the site, and temperature can all influence performance. False alarms may occur, and infrequent signal drops are possible. Skin sensitivity, adhesive issues, and charging schedules require planning. For people using glucose-lowering medications, any adjustments should follow an agreed plan with a healthcare professional. The watch is an aid for awareness, not a stand-alone diagnostic device or an emergency tool.
Privacy and cost deserve attention. Glucose data may sync across devices and cloud services; review permissions and sharing settings to control who sees what. Strong passcodes, timely updates, and cautious use of third-party apps reduce exposure. Costs include the watch itself, potential subscription features, and, if applicable, sensors and supplies. Insurance coverage and regional programs vary, so investigate benefits before committing. Accessibility features—haptics, large fonts, high-contrast faces—can make monitoring more inclusive, especially for those with visual or hearing needs.
If you are choosing a setup, use this practical checklist:
– Confirm compatibility between your watch, phone, and chosen glucose data source.
– Ensure that vibration alerts, glanceable complications, and offline behavior match your routine.
– Calibrate or confirm sensor accuracy as directed, and learn how lag affects decisions during activity or illness.
– Set alert thresholds that balance safety with noise, and enable quiet hours to prevent alert fatigue.
– Plan a simple charging habit to avoid coverage gaps, and keep a backup method for checks when needed.
The right measure of ambition is steady, not heroic. Start with a single goal—fewer lows during commutes, smoother mornings, or calmer workouts—and let wins guide the next step. When glucose becomes glanceable, you shift from reacting to anticipating, which is where confidence grows. For people managing diabetes and those focused on prevention, smartwatch monitoring offers practical visibility and timely nudges, provided it is grounded in clinical guidance and realistic expectations. Treat the watch as your co-pilot: it does not fly the plane, but it keeps critical instruments in view so you can navigate the day with clarity.
This content is educational and does not replace personalized medical advice. Always consult a qualified professional for diagnosis, treatment, and changes to your care plan.